Diabetic foot care in elderly citizens
01-10-24
When a foot's skin tissue deteriorates, exposing the layers of skin below, diabetic foot ulcers form. The burden of foot illness is great for elderly diabetic individuals. Peripheral neuropathy, foot abnormalities, and peripheral arterial disease are the primary causes of foot disease (PAD). Poor vision, irregular gait, limited mobility, and medical co-morbidities are additional risk factors. We can manage diabetic foot problems at several stages using various interventions.
What are the early symptoms?
A diabetic individual might not realize having a diabetic foot ulcer until it has already advanced. The cause of this is that many diabetics do not feel pain from cuts or wounds because of poor circulation and peripheral neuropathy, which causes them to lose feeling in their extremities.
One of the earliest indications of a diabetic foot ulcer is drainage from the incision that discolours the wearer's socks. A diabetic foot ulcer's presence may also be associated by irritation, swelling, or an unpleasant odour. In more serious instances, the skin around the wound may become calloused or uncomfortable to the touch, or a person may detect discolouration (which may be black).
If any of these signs appear, get medical attention right away, ideally from a podiatrist, to stop the wound from getting worse and start any necessary treatments.
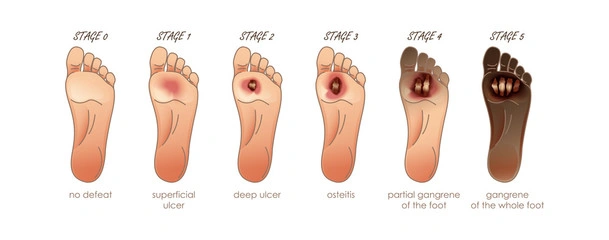
What are the stages?
Diabetes can lead to difficulties if you don't control it with exercise, nutrition, and insulin-based treatments. Foot ulcers are a common consequence. Foot ulcers typically develop under the big toes and on the balls of the feet. Some even develop to where the bone is visible. These ulcers can become very painful, and severe instances could need to be amputated.
Normal
You can suffer inflamed skin, unpleasant foot odour, swelling, or redness in the early stages of a diabetic foot ulcer. Early diabetic foot ulcers frequently feature healed lesions rather than open sores. A foot ulcer may not yet have clear symptoms.
High-Risk
Ischemia, neuropathy, edoema, deformity, and calluses are some of these risk factors at this stage. Most abnormalities can be accommodated with proper footwear. A callus should be aggressively treated because it is a substantial precursor to an ulcer, especially in a foot with neuropathy. These minor cuts go through the epidermis or both the dermis and the epidermis.
Ulcerated
The tendon, joint capsule, or bone are all affected by a deeper foot ulcer in the third stage. These ulcers are frequently linked to wearing inappropriate footwear or suffering from foot damage. Pressure relief, a clean debridement, and dressings are necessary for diabetic foot ulcers in stage 3.
Infected
This includes deeper tissues, and the incision on the foot gets infected. Make sure to check your feet each day, maintain good foot hygiene, remove any extra dirt from the region, microbiological control, and take medications to avoid a condition like this from getting worse. To determine whether you require surgical drainage and debridement, you should consult a foot specialist.
Necrotic
The final stage is when the area begins to necrotize. Wet necrosis and dry necrosis are two different necrosis. Wet necrosis on neuropathic foot causes surgical debridement and intravenous antibiotics. Vascular repair might also be necessary for neuroischemic feet that have wet necrosis. The number of feet that become infected and eventually go necrotic can be decreased with aggressive care. As a result, there are potentially fewer amputations. The foot is heavily gangrenous and it's possible that the entire foot has gangrene. We can avoid this stage by visiting a podiatrist frequently and preserving blood circulation.
How to prevent it?
The prevention of foot ulcers depends on identifying individuals who are at high risk and avoiding situations that could set them off, like:
●wearing uncomfortable shoes,
●going barefoot, or
●Wash your feet with lukewarm water
●Gently dry your feet, specially in between your toes
●Clean your footwear regularly
●Cut your nails regularly
Amputations due to PAD should be avoided by:
●Maintaining lifelong glycaemic control,
●Treating hypertension and dyslipidemia, and
●Quitting smoking.
Foot ulcers are treated by:
●Relieving pressure (off-loading),
●Cleaning the area, and
●Treating ischemia and infection.
It causes a tailored strategy considering the co-morbidities and functional state of the patient. Off-loading is still necessary, but it is rare to use crutches or whole contact casts. However, it is frequently helpful to provide customized standard footwear and insist on its regular use, even at home.
In order to effectively treat foot ulcers, pressure alleviation (off-loading), and wounds, we should compare the advantages of invasive orthopedic or vascular surgery to the dangers of extended hospital stays and the ensuing functional decrease. To lessen the burden of diabetic foot disease in the elderly, preventative efforts and specialized care are required.