Managing Diabetic Retinopathy in the Elderly: Insights, Treatments, and Lifestyle Strategies
01-10-24
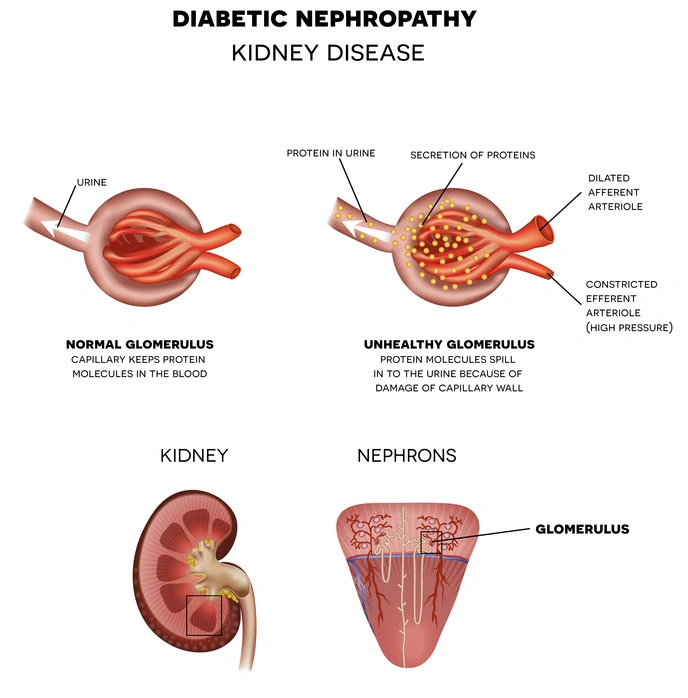
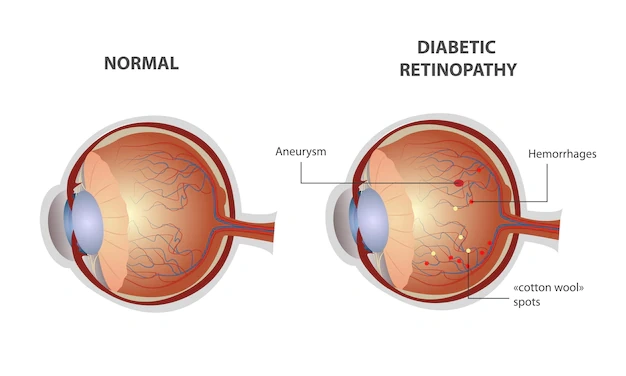
People who have diabetes may develop diabetic retinopathy, an eye disorder that can lead to blindness and vision loss. The retina's blood vessels are affected (the light-sensitive layer of tissue in the back of your eye). The prevalence of both diabetes and its most prevalent consequence, diabetic retinopathy, is rising (DR).
Age-related retinal changes must be considered in order to effectively treat DR in the older population, such as
●reduced blood flow,
●retinal thinning, and
●microglial changes.
These changes can make the retina more susceptible to oxidative and ischemic damage. Given these factors and the pathophysiology of DR, certain pathways, such as the polyol pathway and the vascular endothelial growth factor (VEGF) axis, may be more important in the advancement of DR in aged people.
It's crucial to undergo a thorough dilated eye exam at least once a year if you have diabetes. Although diabetic retinopathy may not initially present with any symptoms, detecting it early might help you take precautions to preserve your vision.
This retinopathy frequently coexists with certain elderly ophthalmological conditions (cataract, glaucoma, age-related macular degeneration [ARMD]). Several eye issues, including the rise in senior diabetic patients and the decline in ophthalmologists, combine to make the problem worse.
Treatment may include:
●intravitreal corticosteroids,
●intravitreal anti-VEGF medicines,
●laser photocoagulation,
●Systemic medications, and
●surgical procedures.
It is crucial to consider how pharmacokinetics and pharmacodynamics alter with age when taking treatments; oral drug absorption can decline, and ocular drug metabolism may impact affecte and administration strategies. Elderly people are more prone than younger patients to miss visits or follow their prescribed treatment plans, and anti-VEGF drug undertreatment frequently results in less than ideal results.
Understanding how aging affects disease progression, medication metabolism, and adherence is essential for ensuring that this population receives proper care as the number of older DR patients rises.
LIFESTYLE MANAGEMENT
A healthy lifestyle can help patients prevent visual abnormalities and long-term vision loss, and complement treatment for diabetic retinopathy. Patients with diabetic retinopathy should take into consideration the following lifestyle modifications:
Adopt a healthy diet:
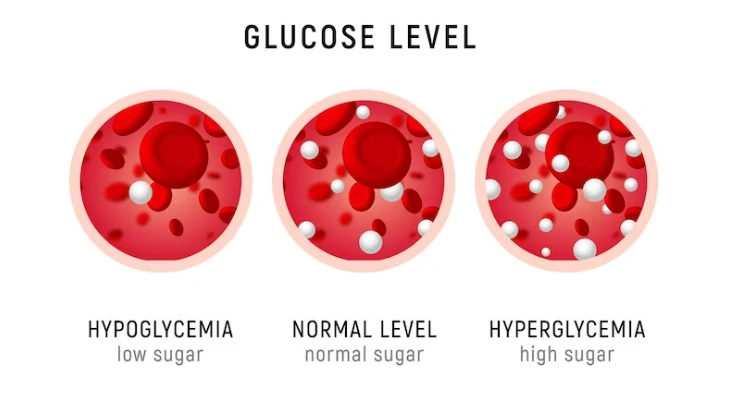
The biggest influence on blood sugar levels comes from a person's food. It's critical to pay attention to the nutrients that the body is consuming. Meals ought to contain a balanced serving of protein, veggies, and fruits. Patients with diabetes should attempt to limit their intake of empty calories from junk food and sweets.
Get active:
Everyone should strive for at least 30 minutes of activity three to five times a week. Patients with diabetes can benefit from this healthy habit. Exercise reduces blood sugar by boosting the body's utilization of glucose. Patients can maintain a healthy weight by following a healthy diet and engaging in regular exercise. These behaviors are strongly advised for diabetic patients because obesity is a major risk factor for diabetic retinopathy.
Avoid smoking:
Another bad habit that raises the risk of diabetic retinopathy is smoking. Anyone with diabetes who smokes or uses tobacco products should it up.
Seek routine medical attention:
Diabetic people should routinely visit their primary care physician and an eye doctor. These regular check-ups enable early detection of any potential diabetic problems, enabling rapid treatment.