All you need to know about Coronary artery disease
28-09-24
What is coronary artery disease?
When the main blood vessels that supply the heart with blood, oxygen, and nutrients become injured or ill, coronary artery disease (CAD), also known as coronary heart disease (CHD), occurs. The bigger coronary arteries on the surface of the heart are affected by coronary artery disease. The microscopic arteries in the heart muscle are impacted by coronary microvascular disease, another type of heart condition. Women are more likely to have coronary microvascular disease.
CAD is one of the leading causes of mortality in both women and men older than 65 years. Seniors are more likely to get affected by CAD than the young population.
In India, coronary heart disease (CHD) is an epidemic and one of the leading causes of illness, mortality, and disease burden in seniors. A heart-healthy lifestyle can help most seniors avoid coronary heart disease. If you have coronary heart disease, your condition may require medication, surgery, lifestyle modifications that promote heart health, or a combination of these treatments.
What are the symptoms of CAD?
Initial symptoms could not be seen, or they might only show up when the heart is pumping rapidly, such as during exercise in seniors. Less and less blood reaches the heart as the coronary arteries constrict, and symptoms in elders may worsen or occur more frequently.
Signs and symptoms of coronary artery disease among seniors can include:
Chest pain (Angina)
Your chest may feel tight or under strain. Some claim that the sensation is similar to having someone stand on their chest. The middle or left side of the chest is the main location for chest pain. Angina can be brought on by exertion or intense feelings. The pain typically disappears minutes after the triggering event is over. Some people, especially women, may have transient or acute pain in the neck, back, or arm. In most situations, chest pain may not be experienced by seniors who are suffering from CAD.
Difficulty in breathing
This is one of the major symptoms in seniors. You can experience difficulty breathing. The heart strains to pump enough blood to meet the needs of the body as the need for oxygen-rich blood rises. Breathing difficulties or acute exhaustion after effort could result from this.
Fatigue
You may experience unusual fatigue if the heart is unable to pump enough blood to meet your body's requirements.
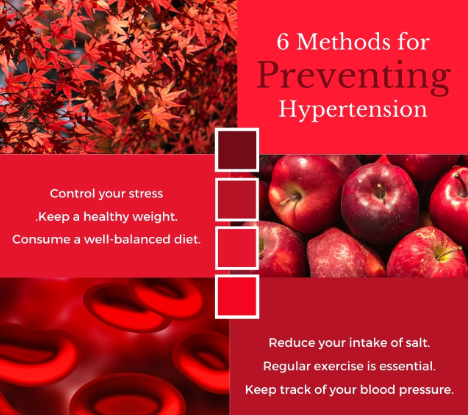
Heart attack (Myocardial Infarction)
A heart attack is brought on by a totally clogged coronary artery. Chest discomfort or pressure, shoulder or arm pain, breathlessness, and perspiration are the typical indications and symptoms of a heart attack. Women may experience less common symptoms including neck or jaw pain, tiredness, and nausea. Some heart attacks don't result in any observable symptoms or indicators.
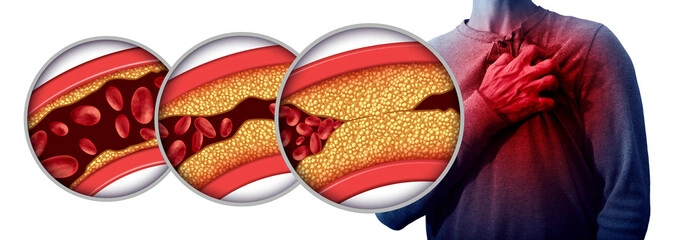
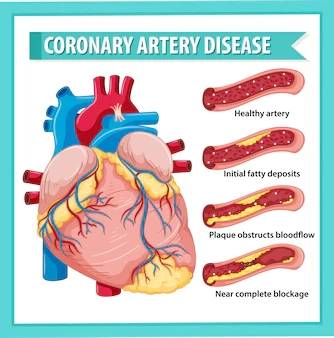
What are the causes of CAD?
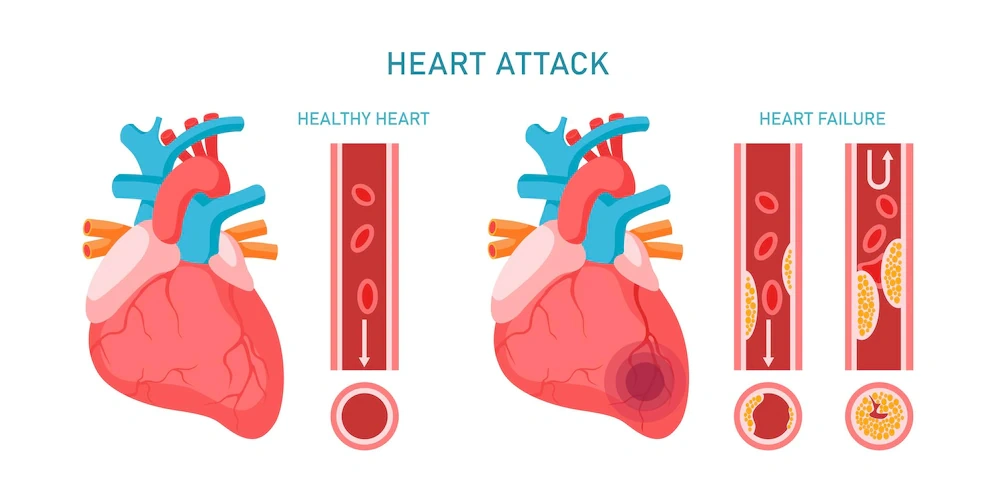
Plaque, which is a cholesterol-containing deposit, frequently causes CAD. It is a waxy substance made up of a mixture of cholesterol, fat, and other chemicals that adheres to the blood vessel walls. A condition known as atherosclerosis may result as a result of the gradual hardening and narrowing of the arteries. Chest pain, shortness of breath, and other symptoms of coronary artery disease are eventually brought on by the narrowing of coronary arteries brought on by plaque formation in seniors. In the elderly population, a heart attack may be brought on by uncontrolled coronary artery disease or a total blockage of arteries.
Coronary artery disease develops gradually over time and may go undiagnosed until plaque buildup causes a blocked artery in the heart, which causes a heart attack. Following a healthy lifestyle can help avoid the illness, and regular health checks can help discover it early.
Vascular damage to the inner layer of the coronary artery brought on by the accumulation of plaque is the most frequent cause of coronary artery disease. There are many potential causes of the harm in elders, including:
●Sedentary kind of life
●Either insulin resistance or diabetes
●Elevated blood pressure
●High triglycerides
●Smoking
What are the risk factors of CAD?
The number of risk factors you have and how significant they affect how likely you are to develop coronary heart disease. Changing to a heart-healthy lifestyle can alter some risk factors, such as high blood pressure and high cholesterol. You cannot change other risk factors, such as your sex, advanced age, family history, race, or ethnicity.
1.Age
In seniors, as they age, plaque builds up in the arteries due to genetic or lifestyle factors.
Around the age of 45, the risk of coronary heart disease in males begins to rise. Women are less likely than men to develop coronary heart disease before menopause. The risk increases for women after the age of about 55. This is probably due to estrogen levels in women declining after menopause.
2.Environment and occupation
Other disorders like atherosclerosis and high blood pressure that are known to raise the risk of coronary heart disease in seniors may also be brought on by or made worse by air pollution.
Your risk at work could increase if you:
●They are subject to contaminants, radiation, or other dangers
●Stressed out a lot at work
●Sit for a long time
●Work more than 55 hours per week, or irregular, long, or late shifts that interfere with your sleep
3.Family history and genetics
This is one of the risk factors for coronary heart disease. This is particularly true if your mother, sister, or father were diagnosed prior to age 65 or prior to age 55, respectively.
4.Lifestyle habits
Unhealthy lifestyle choices eventually raise your risk of coronary heart disease because they might cause plaque to accumulate in the blood arteries of the heart.
●Inactivity: Physical inactivity can make other heart disease risk factors worse, including high blood pressure, diabetes, prediabetes, high blood cholesterol, and triglyceride levels, as well as overweight and obesity.
●Inadequate sleep: The chance of developing coronary heart disease may increase if seniors don't obtain enough sleep of a high caliber, or if you wake up frequently at night. Your heart rate and blood pressure decrease as you sleep. Compared to while you are awake, your heart does not beat as quickly. Your heart rate and blood pressure rise to the same levels as when you are awake and relaxed as you start to wake up. Angina and heart attacks have been connected to abrupt awakenings because of the fast rise in blood pressure and heart rate that can occur.
●Cigarette: The blood vessels can be harmed by smoking or prolonged exposure to secondhand smoke in seniors.
●Stress: Your arteries may constrict as a result of stress. If stress increases your likelihood of smoking or overeating foods heavy in fat and added sweets, it may also indirectly increase your risk of coronary heart disease among elders.
●Unhealthy eating: Habits such as consuming a lot of refined carbs and saturated fats (such as white bread, pasta, and rice) can cause obesity, overweight, high blood cholesterol, atherosclerosis, and plaque accumulation in the arteries of the heart.
5.Other medical problems
Existing medical ailments may become the major risk factor in seniors. So, it is always important to stay as healthy as possible.
Some of these ailments include atherosclerosis, hypertension, high cholesterol, chronic kidney disease, diabetes, AIDS, metabolic syndromes, overweight, obesity, autoimmune conditions, sleep disorders, mental health issues, and others. The chances of getting affected with CAD can be minimized by following regular medications for the existing disease.
6.Ethnicity or race
The second leading cause of death among Hispanics, Asian Americans or Pacific Islanders, American Indians, or Alaska Natives is heart disease. Compared to other Asian Americans, those of South Asian heritage had a higher risk of coronary heart disease and significant consequences.
7.Gender
Both genders are affected by coronary heart disease. Men are more frequently affected by obstructive coronary artery disease. However, women are more likely to have non-obstructive coronary artery disease.
Ask your doctor about testing to look for non-obstructive coronary artery disease or coronary microvascular disease if you are a woman experiencing chest discomfort or shortness of breath after physical exertion.
What are the tests performed?
Consulting your doctor based on the symptoms may help in the early diagnosis of the disease. Additionally, it's possible that your doctor will request blood tests to evaluate your levels of proteins, sugar, lipoproteins, triglycerides, cholesterol, and other markers of inflammation. Your medical history and any symptoms you may be experiencing will probably be discussed.
The following tests are used to detect or track coronary artery disease:
An electrocardiogram (EKG or ECG) can be used to assess the regularity or irregularity of the heart's rhythm. Additionally, an EKG documents the frequency and timing of electrical signals that go through the heart.
Calcium scan of the heart
It calculates the calcium content of your coronary artery walls. This exam is a particular kind of cardiac CT scan. Coronary calcium scans can also be used to determine a person's risk of developing coronary heart disease for smokers or people with no symptoms.
Stress tests
This provides both diagnostic and prognosis assessments in seniors. It examines how your heart responds to physical strain. To make your heart work hard and beat quickly during a stress test, you either pedal a stationary bike or walk or run on a treadmill.
Heart MRI (magnetic resonance imaging)
It finds issues with blood flow in the heart or coronary arteries or tissue damage. It can aid your doctor in the diagnosis of nonobstructive or obstructive coronary artery disease as well as coronary microvascular disease. Cardiac MRI can also assist in interpreting the findings of other imaging examinations.
Positron emission tomography (PET) of the heart
It evaluates blood flow into the cardiac tissues and through the tiny coronary blood channels. A nuclear heart scan of this kind can identify coronary microvascular disease.
Angiogram of the heart
It displays your coronary arteries' interiors. Your doctor will use a process known as cardiac catheterization to insert the dye into your coronary arteries. If other tests indicate that you are likely to have coronary artery disease, this procedure is frequently utilized.
Computed Tomographic (CT Scan) angiography of the heart
Instead of invasive cardiac catheterization, this imaging procedure (scanning) reveals the interior of your coronary arteries.
What are the treatments available?
Medical therapy, along with lifestyle modifications and the treatment of CAD risk factors, is the primary mode of treatment for most elderly patients. Some medications can treat other medical disorders that may be associated with coronary heart disease, as well as lessen or stop chest pain.
●The blood pressure and heart rate are both lowered with ACE inhibitors and beta blockers.
Eg: Atenolol
●Calcium channel blockers cause blood arteries to relax, which lowers blood pressure.
Eg: Amlodipine
●If you have both coronary heart disease and diabetes, blood sugar-controlling medications including empagliflozin, canagliflozin, and liraglutide can help reduce your risk for problems.
●If you have diabetes, metformin prevents plaque development.
●Nitrates widen your coronary arteries and lessen or stop angina-related chest pain.
Eg: Nitroglycerin
●Ranolazine treats chest pain that may result from the coronary microvascular disease.
●Statin and non-statin therapy: Treatments that don't involve statins can lower high blood cholesterol. If you have diabetes and are between the ages of 40 and 75, you may need statin therapy due to your increased risk of coronary heart disease or stroke.
Eg: Atorvastatin
●Non-statin therapy: When statins are ineffective or have unwanted side effects, non-statin therapy may be used to lower cholesterol. The non-statin medications ezetimibe, bile acid sequestrants for lowering cholesterol, or fenofibrate for lowering triglycerides may also be prescribed by your doctor. Omega-3 fatty acids may also be suggested for your healthy diet.
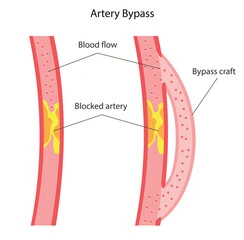
Surgeries or other procedures
To treat more severe coronary heart disease, you might require treatment or heart surgery.
●By removing plaque buildup, angiography widens or unblocks blocked or restricted coronary arteries. After angiography, a tiny mesh tube known as a stent is typically inserted to stop the artery from narrowing again.
●By using healthy arteries from the chest wall and veins from the legs to bypass the obstructed arteries, bypass surgery improves blood flow to the heart. Patients with significant coronary artery disease in numerous coronary arteries are frequently treated with bypass surgery by surgeons.
●When other treatments are either too risky or ineffective, severe angina associated with coronary heart disease is treated with laser surgery.
What are the necessary healthy lifestyle modifications?
Lifestyle modifications are intended to stop further plaque buildup and lessen blood vessel damage. Some actions might even assist in lowering the level of plaque in your blood vessels. Additionally, lowers your risk of stroke and heart attack, through these adjustments.
Aim to maintain a healthy weight
You can manage several coronary heart disease risk factors, such as high blood cholesterol and diabetes, by losing merely 3 to 5 percent of your present body weight. Additionally, greater weight loss can lower blood pressure measurements.
Be active physically
Regular exercise can help control coronary heart disease risk factors such as high blood pressure, high cholesterol, and obesity. Your body undergoes many changes as you age. So, before beginning any fitness regimen, find out your current physical condition. Do some research on the degree of physical activity for you before beginning any workout regimen.
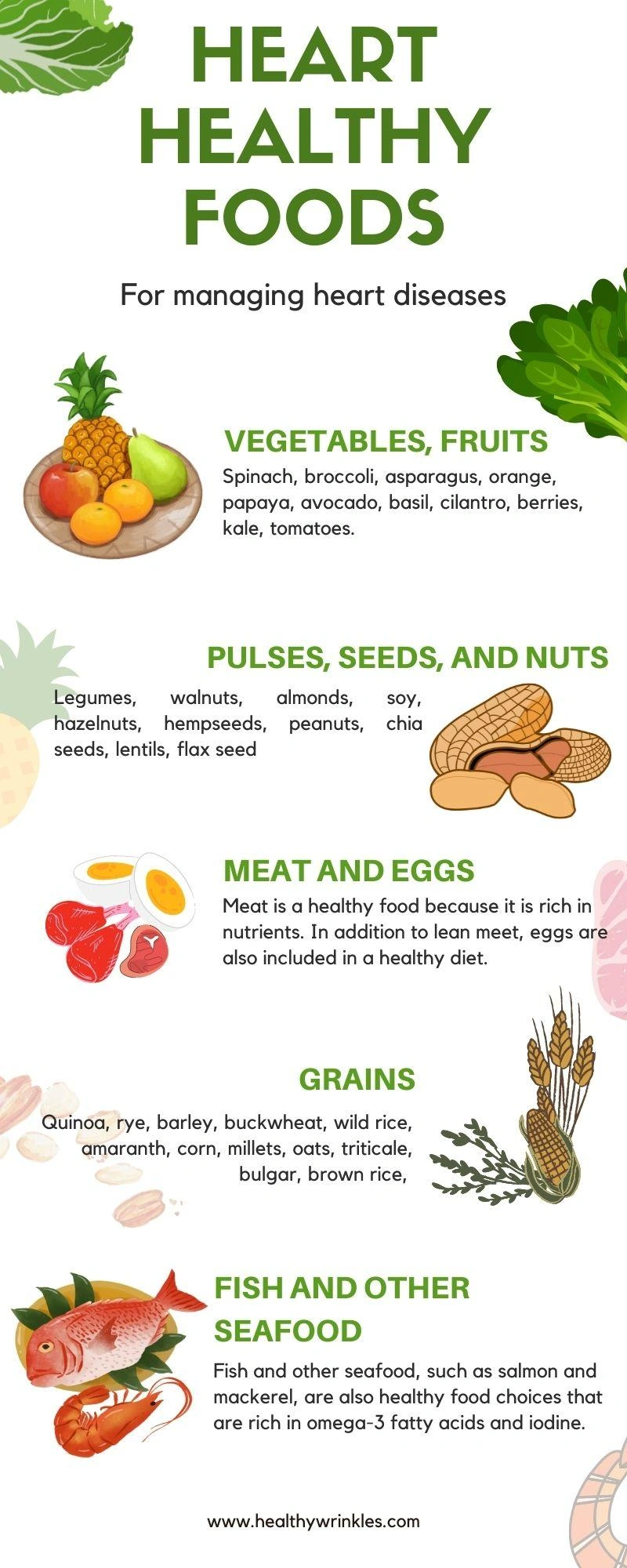
Healthy diet
The DASH (Dietary Approaches to Stop Hypertension) eating plan is one example of a heart-healthy diet. Fruits, vegetables, and whole grains are part of a heart-healthy diet, which also restricts saturated fats, sodium (salt), added sweets, and alcohol.
Stress management
Your emotional and physical well-being can be enhanced by learning how to control your stress, unwind, and deal with issues in your elder age.
Give up smoking
Smoking causes damage to your blood vessels and lung tissue, lowers the oxygen content of your blood, and makes your heart beat more quickly. Keep in mind that passive smoking might be dangerous as well. If at all possible, avoid being around cigarette smoke.
Reduce or stop drinking alcohol
Alcohol consumption in excess raises blood triglyceride levels, which help to cause heart arrhythmias and atherosclerosis. Alcohol and some drugs may interact.
For men, moderate drinking is defined as 2 drinks or fewer per day, and for women, it's 1 drink or fewer per day.
Adequate sleep
Most seniors find it difficult to sleep because of various reasons. But, it is very important to have a sound sleep for a healthier you. Elders should get between 7 and 9 hours of sleep per night.
Take the prescription drugs you were given as directed. Follow the directions on the label or the advice of your doctor while taking drugs. If you have any concerns regarding usage or adverse effects, speak with your doctor.
Keep in regular contact with your medical team, follow your treatment plan, and attend all scheduled appointments. Maintaining constant communication with your medical staff can help you in managing the disease.