Antibiotic-resistance-in-seniors
28-09-24
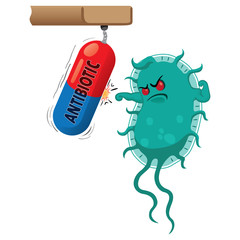
Antibiotic resistance is one of the global leading problems facing medicine as many micro-organisms are developing resistance to antibiotic they were previously sensitive to. This has a significant impact on health care.
Use of Antibiotics in the Elderly
Antibiotics are the most commonly used and misunderstood agents, contributing to the massive global problem of loss of efficacy due to resistance. Antibiotic misuse is the primary cause of antibiotic resistance. When antibiotics are taken, only bacteria that are susceptible to the antibiotic are killed; resistant bacteria are not killed.
Elderly Antibiotic Resistance
Improper antibiotic prescribing practises may result in the unnecessary use of antibiotics, contributing to the spread of resistant bacteria.
Antibiotic resistance is a problem in nursing homes, as infections caused by multi-resistant bacteria are becoming more common among nursing home residents. As a result of antibiotic use in these long-term care facilities, nursing homes for the elderly serve as reservoirs for antibiotic-resistant bacteria strains. Pathogens that are multidrug resistant are frequently recovered in these long-term care facilities.
In nursing homes, anatomical and physiological changes caused by ageing, as well as the use of urinary catheters, nasogastric and percutaneous feeding tubes, and intravenous catheters, all predispose the elderly to bacteria colonisation and infections.
Effects of Antibiotic Resistance
●Antibiotic Resistance has a negative impact on treatment failure because the microorganism(s) are no longer susceptible to the antibiotic.
●There is more disability as a result of illness and death.
●Due to treatment failure, there is a prolonged hospital stay.
●There is a greater financial outlay for treatment costs.
Antibiotic Resistance Prevention in the Elderly
●Antibiotic resistance in the elderly cannot be completely avoided.
●Keep infections from spreading and transferring antibiotic-resistant strains.
●Antibiotic-resistant strains should be tracked.
●Antibiotics tablet should be used only when absolutely necessary, which necessitates antibiotic training and retraining for physicians. Antibiotics medicine should be used in response to culture and sensitivity reports, as well as when the patient exhibits symptoms.
●Research and development of new antibiotic
●Narrow spectrum antibiotics should be used instead of broad spectrum antibiotics because they are more effective against specific microorganisms.
Conclusion
Antibiotic resistance is common, especially among the elderly. Preventive steps should be followed as it has a negative impact on these senior citizens who are predisposed to it, particularly those in long-term care facilities.